ECG vs EKG is a little bit confusing for those who are not in the medical field. It is interesting to learn that despite their alphabetical difference of ‘K’ in ECG vs EKG there is something more different about their word origin but this medical term signifies the same test. Though they are coined differently both ECG and EKG resemble the same meaning. ECG /EKG is a type of medical test that is used by medical professionals as a diagnostic tool for detecting the electrical activity of the heart.
It is a simple medical test that records the electrical activity/ impulse of the heart over a period of time, assesses cardiac health, monitor, and detect heart abnormalities, and produce the rhythm of the heart visually.
In this comprehensive article, we will explore the world of ECG, covering the basics, to advance, its numerous benefits, and putting light on its common and essential uses.
Whether you are an individual looking to understand ECG or a medical professional seeking to refresh your knowledge of ECG, you’re in the right place. Let’s explore a journey to reveal the facts about it and appreciate its clinical role in the world of cardiac health.
Difference between ECG vs EKG
ECG: It stands for ‘electrocardiogram’. This term is derived from the German term “Elektrocardiogram” This term is commonly used in many parts of the world like Asia and Europe.
EKG: EKG also stands for “Electrocardiogram”.It is derived from the German term “Elektrokardiographie.” The alphabetically different ‘K’ in EKG represents the term “cardiograph”.
Significance of ECG:
- Detection of Heart Abnormalities: It works by analyzing the electrical patterns of the heart. Analyzing the heart’s rhythmic pattern diagnoses different heart abnormalities like Myocardial infarction(MI) and Arrhythmias including atrial fibrillation, atrial tachycardia, bradycardia, and ventricular tachycardia. In myocardial infarction, It shows
- ST- elevation
- T-wave inversion
- Pathological Q wave
- Monitor Cardiac Health: In the assessment of the overall cardiac health of the patient, it is very significant. From evaluating the size of the heart to studying structure, and function, and providing ideas for the diagnosis and management of heart diseases.
- Assess treatment protocol: it is a proven diagnostic tool for cardiac health. The report is used for treatment, prescribing medications, and sometimes recommending surgical interventions as needed.
- Monitoring patients in Intensive care: It is used for continuous monitoring of patients in the intensive care setup for critically ill patients. It helps to track changes in heart rhythm and function over time.
Overall, The significance of the ECG is a widespread technologically advanced tool that provides accurate data on the human heart, assesses the rhythmic patterns of the heart detects any abnormal rhythm or abnormalities, and guides patients’ condition to health care professionals. It is a great asset in the medical field especially in the cardiac sectors.
Cycle of heart
There is a working cycle of the heart known as the cardiac cycle. The cardiac cycle is the series of cardiac events that occur from the beginning of one heartbeat to the beginning of another heartbeat. Contraction and relaxation occur during this phase. The period of contraction is systole and the period of relaxation is diastole.
Conducting system of the Heart /Hearts electrical system
The cardiac cycle is generated by the impulse generated by the Sinoatrial node (SA) which is known as the pacemaker of the heart. The complex networks of specialized cells and fibers generate and regulate the electrical signal responsible for the coordination of the heartbeat. The cardiac cycle is controlled by the electrical impulse brought by the conducting system of the heart. However cardiac cycle is under modulation by the cardiac centre medulla oblongata.
Here’s an explanation of the key components and processes of the heart’s electrical system
- Sinoatrial node
- Atrioventricular node
- Atrioventricular bundle
- Purkinje Fibers

SA Node: There is a mass of specialized types of cells in the wall of the right atrium of the heart. The mass is present near the opening of the superior vena cava. It is also the pacemaker of the heart. It normally initiates the impulse more rapidly than any other neuromuscular cell. Atrial walls pass the impulse and cause the atria to contract simultaneously at the same time it reaches to AV node. It generates the impulse at the rate of 70/min.
AV Node: It is smaller than the SA node and lies in the lower and dorsal part of the atrial septum just nearer to the atrioventricular valve. It receives the impulse from the sinoatrial node however it is itself capable of generating the impulse but at a slower rate than the SA node. It generates impulse at the speed of 60/ minutes.
AV Bundles: There is a mass of specialized fibers originating from the AV node passing into the top of the ventricular septum and then dividing into the left and right branches. It carries the impulse from the atria to the ventricles.
Purkinje Fibres: It arises by the division of right and left bundle breakdown into fine fibers called Purkinje fibers. It carries the impulse to all parts of the ventricle where ventricle contraction occurs pumping the blood into the pulmonary artery.
How ECG works
A diagnostic test electrocardiogram records the electrical activity of the heart. It works by using electrodes, multiple leads, and signal-recording equipment. Here’s how ECG works.

- Electrodes: ECG electrodes are small, and adhesive patches that are placed on specific areas of the body like limbs and chest to detect the electrical signals generated by the heart. Typically, 10 electrodes are in use for a standard ECG. These electrodes are placed in specific locations:
- Limb Leads: There are 4 electrodes placed on the limbs two on the wrists (left and right) and two on the ankles (left and right). These electrodes are labeled as RA (Right Arm), LA (Left Arm), RL (Right Leg), and LL (Left Leg).
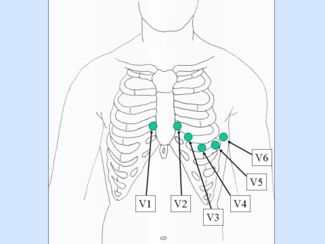
- Chest Leads: The remaining six electrodes are placed on the chest area, allowing for the recording from different views of the heart. These chest leads are positioned at specific locations on the chest wall and are labeled as V1, V2, V3, V4, V5, and V6. They are placed in the following anatomical location in the chest.
ECG leads placement
- V1: In the fourth intercostal space just to the right of the sternum.
- V2: In the fourth intercostal space just to the left of the sternum (mid-clavicular line).
- V3: In the fifth intercostal space between V2 and V4, midway between their positions.
- V4: In the fifth intercostal space at the mid-clavicular line in the left anterior axillary line.
- V5: At the same level as V4 but slightly in the left mid-clavicular line.
- V6: In the left mid-axillary line at the same level as V4 and V5.
Slippery conductive jelly in the leads to comfort the patients from metallic leads and to improve the quality of electrical signal transmission between the skin and the ECG electrodes.
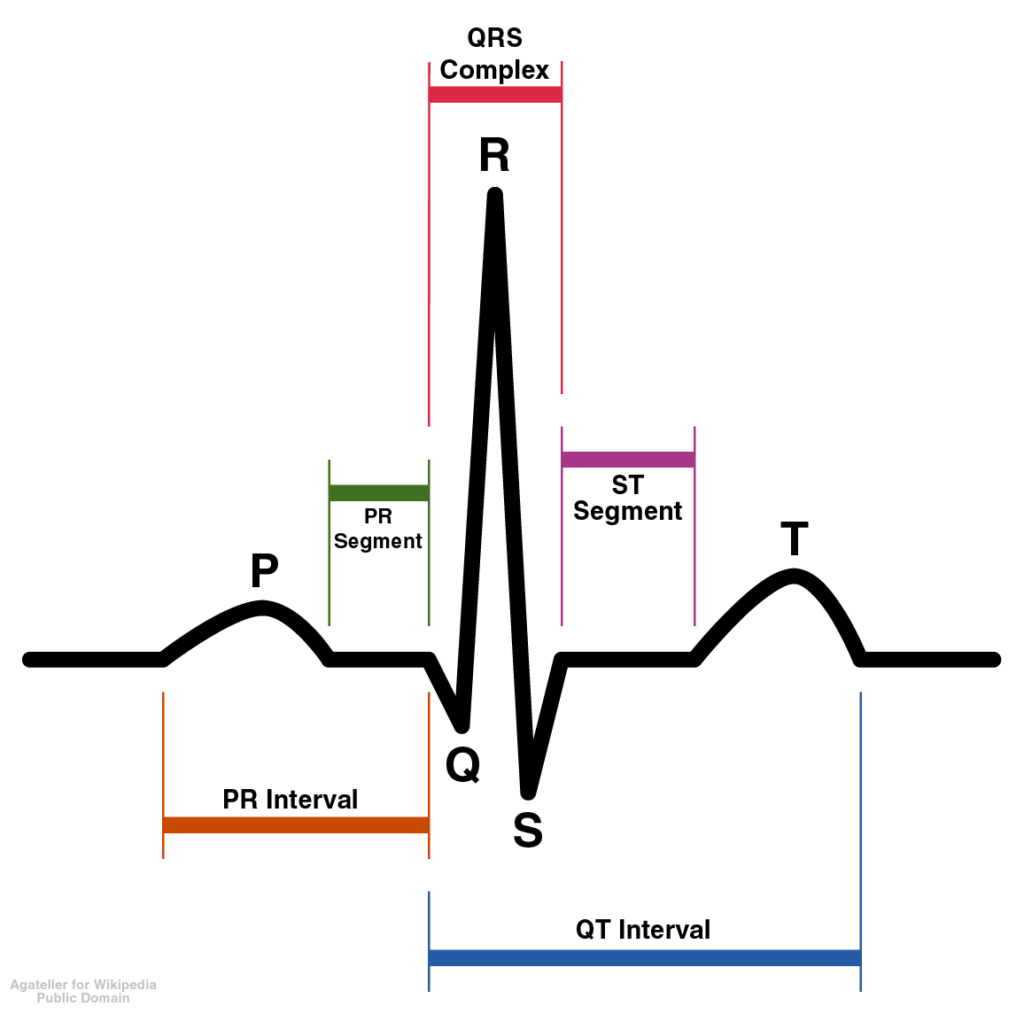
Once the electrodes are properly placed on the wrist, ankle, and chest, they detect the electrical signals produced by the cardiac electrical activity. As the heart contract and relax the depolarization and repolarization signal of the heart’s chamber are recorded. These electrodes are connected to an ECG machine which measures the electrical activity. Each lead provides a unique perspective of heart functions from different angles. The electrical signals are then shown digitally on screen and can be printed on graph paper. The wave consists of the following significance.
- P-Wave: Represents atrial contraction.
- QRS Complex: Represents ventricular contraction.
- T-Wave: Represents ventricular relaxation.
The recorded ECG is interpreted or analyzed by a cardiologist or technician for any abnormalities.
Common Abnormalities seen in ECG
Common abnormalities detected in an Electrocardiogram (ECG or EKG) are key indicators of cardiac health and can provide crucial information for diagnosing and managing heart conditions. Here are some common ECG abnormalities.
- Atrial Fibrillation: The irregular and rapid atrial contractions, leading to an irregular heart rhythm leading to a high risk of stroke, heart failure, and other complications is Atrial fibrillation.
- Ventricular Tachycardia: Fast and potentially life-threatening rhythm originating in the ventricles.
- Ventricular Fibrillation: It is a mixed and uncoordinated rhythm of the ventricles which is a medical emergency and can result in cardiac arrest and death if not treated immediately.
- Bradycardia: It is an abnormally slow heart rate below 60 per minute. It can lead to dizziness, fainting, and reduced cardiac output.
- Prolonged QT Interval: A prolonged QT interval can increase the risk of life-threatening arrhythmias, particularly Torsades de Pointes.
- ST- Elevated Myocardial infarction (STEMI): ST-segment elevation indicates myocardial infarction (heart attack) with ongoing damage to the heart muscle. Immediate intervention is necessary to restore blood flow to the affected artery.
- ST-Segment Depression myocardial infarction [NSTEMI]: ST-segment depression can indicate unstable angina suggesting reduced blood flow to the heart muscle. These conditions require prompt evaluation and treatment.
- T-Wave Inversions: T-wave inversions are found indicators of myocardial ischemia, injury, or other cardiac abnormalities.
It’s important to properly analyze ECG abnormalities before making the diagnosis. Proper interpretation in relation to a patient’s clinical history, symptoms, and other diagnostic tests.
Step-by-step ECG procedure.
The Electrocardiogram (ECG or EKG) procedure is a non-invasive test and easy to perform. It typically takes just a few minutes to complete. Here’s a step-by-step explanation of the ECG procedure:
- Explain the procedure to the patients and get consent from the patient.
- The patent is asked to remove any clothing, jewelry, or electrical device like mobile phones, watches, or any other metallic substance to avoid errors.
- The patient is positioned comfortably on an examination table or bed.
- The electrodes are attached to specific areas of the body. For a standard 12-lead ECG, ten electrodes are typically placed on the following locations.
- Four electrodes on the limbs: Two on the wrists (right and left) and two on the ankles (right and left). They are usually with color labels as Black, Red, Yellow, and Green.
- Six electrodes on the chest: These are positioned at specific locations on the chest wall and are labeled V1, V2, V3, V4, V5, and V6.
- Gelly is applied in small amounts for good electrical conductivity and electrodes are placed manually.
- Before recording samples of the waves are calibrated to ensure accurate measurements. Confirming that the electrical signals are being transmitted correctly.
- Once everything is set up, the ECG recording begins. During recording patient is asked to remain still and breathe normally. Any movement or muscle tension can interfere with the accuracy of the ECG.
- ECG recording is then monitored by a technician to ensure that all leads are providing clear and consistent signals. If errors are seen adjustments are made to lead connections to improve signal quality.
- The electrical activity of the heart in a series of waveforms on graph paper is printed.
- Once the ECG is complete, the electrodes are removed and the gel on the skin is wiped off with tissue.
In conclusion, the Electrocardiogram (ECG) is a proven great asset in modern medicine in the field of cardiology, offering deep study into the heart’s electrical activity. Its non-invasive nature, speed, and accuracy make it a great asset in diagnosing and monitoring a wide range of cardiac conditions, ultimately saving lives and improving patient outcomes.
